Anna-Carin Fagerlind Ståhl shows how dangerous myths have evolved that protect government and business from accountability for bad employment practices.
Author: Anna-Carin Fagerlind Ståhl
Work is health promoting, provides meaning and a context to the otherwise unstructured and socially isolated human existence; work is an opportunity for autonomy and independence, a road out of poverty and illness – or so we are told by scientific publications, health care and welfare policies alike.
At the same time there is an unquestionable association between work and ill health, especially the common mental disorders that include depression, anxiety and exhaustion or burnout.
Figure 1. The Wonderful Wonderland of Work*
This article will summarise the research about the association between work and common mental disorders – what we can say on the subject - beyond reasonable doubt. It will do so by examining certain assumptions that are as popular in the academic context as they are in politics and the media; assumptions that are simplifications of reality with the purpose of making the too complex simpler and the disturbing more comfortable: myths. Finally, the potential consequences of this mythology will be discussed.
‘Work’ will refer to the investment of time (and sometimes energy) in return for money. ‘Common mental disorders’ refers to symptoms of depression, anxiety, exhaustion or burnout.
As a newly graduated psychologist, I wished to prevent mental illness rather than merely attempt to cure it. The area of work and organizational psychology appeared to provide such possibilities. As a PhD-student on the subject, I realised that no one wanted another thesis about the work-related risks for mental ill health such as burnout: the knowledge already existed in abundance.
We know about the risks.
Still hoping to encourage employers to a more health promoting organization of work I took a more positive approach and identified conditions for health, motivation and performance in my doctoral thesis. A year after my dissertation, the high demands, job insecurity and lack of reward provided at the university took their toll I hit the wall with the symptoms of burnout we knew so much about how to prevent. Returning to work a couple of months later, in accordance to the regulations of the Swedish social insurance system, I did my best to avoid the work that seemed to suffocate me to fellow researchers in Canada where I utilised the data material from my dissertation and wrote an article on the risks for burnout.
As I prepared my research on motivation, as well as burnout, I frequently come across several arguments that I have come to call “myths”. These myths have consequences for how we see “work” and for the prevention of common mental disorders. The greatest victims of this mythology are the employees: who are told that the intensive, effective and lean work process is not harmful and can even be motivating, that mental health such as burnout really is not about the work environment but about the life outside work and how we ‘choose’ to think, feel and behave – and that illness thus equals failure.
Reviews and meta-reviews confirm that the risk for future depression, anxiety and exhaustion/burnout increases with certain aspects that are determined by the way that work is organised. [1, 2]
Hence, work is only as good for health and well-being if the work conditions are health promoting.
Furthermore, work is only as good for health and well-being as the alternative is bad. Sick leave and unemployment are well established risks for health and situations of insecurity, exclusion and stigma. This is not because these situations are inherently evil, but because we have made work an essential source of money and social security, for the majority. Welfare policies are to a higher and higher degree designed to push individuals into employment using strict, demanding and humiliating regulations with means-testing and conditionality.
Scientific reports about work and health do conclude that work is good for health and well-being under the condition that the work environment and the conditions for employment are health promoting, and that it is health promoting in comparison to the health adverse effects of unemployment and sick leave. [3, 4] However, the message appears to often be simplified into the more comfortable myth that “work is good for health and well-being” which among other things justify forcing unemployed and ill people into work without consideration of the actual conditions of that work.
When I present research on work conditions and health, I am almost always confronted by the protests that high demands cannot always be a risk since some like it when there is a lot to do. Cannot demands for high work pace or complex cognitive effort also be motivating? And, even if high demands do constitute a risk, cannot the good social climate we experience at our work place, or some other positive aspects, buffer any potential negative effects on health?
Commonly utilised models describing associations between the work environment and mental health and well-being include hypotheses about motivation and learning in the presence of high demands (see Figure 2).
Perhaps it is because the central assumptions of these models have been confirmed beyond doubt (the health-adverse effects of high demands, low control and other work-related resources) that also their less investigated hypotheses are taken as truths without consideration for the research in support or against them.
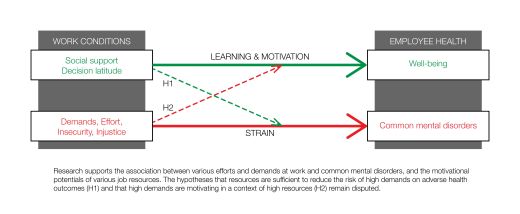
Figure 2. Risks for ill health and resources for well-being
In Figure 2 (a) refers to the well-established association between various risks in the psychosocial work environment and (b) to associations between resources and well-being (c) illustrates the hypothesised motivational process and (d) the buffer-hypothesis.
The idea is that high demands combined with a high degree of control, social support, good leadership or some other ‘positive’ aspect of the work environment will give the individual the ability to overcome the demands, without experiencing strain or negative effects on health, and even experience motivation and joy, being immersed in the activity. This experience of ‘flow’ or work engagement may in addition result in learning: as you successfully cope with high demands, they stop being challenging, and since the experience was intrinsically rewarding you will seek out new challenges (i.e. take on higher demands).
The research on the promotion of positive emotions and subjective well-being at work is not as abundant as the research focused on the risks for mental ill health. Investigating the conditions that were associated with experiences of work enjoyment and motivation in 10 organisations, including over 3,000 employees, we found that it was not the high demands that were motivating or promotive of learning. [5] Rather, having control and being able to decide how to work and able to use skills, alone or in a trusting and helpful social environment at work were associated with experiences of motivation, work engagement and learning. In such an environment, where there are resources rather than demands, individuals are able to be productive and creative, alone or together in the work group, enjoy themselves, solve problems and be creative.
Scrutinising the research on the area it became clear that the idea of motivating demands is a myth. Yes, some like when there is a lot to do and it is likely that a desire for creativity and productivity is inherent in the human nature – but is it the demands for a high work pace and high effort mandated from someone who have power over you that is motivating and conducive for learning and development or is it having opportunities for creativity and performance in a trusting environment? However, the myth is comfortable for organisations aiming to improve efficiency and continuously reducing “wasteful” steps in the work process.
When I couple of years later focused my research on the risks for exhaustion, I took for granted that the association between high demands and future symptoms of burnout would be buffered by job resources such as decision latitude and social capital. The results showed us however that the symptoms of burnout increased depending on how high demands employees experienced – irrespective of their control over decision and skill use or the quality of the social climate at work. [6] There is indeed very little research of high quality that supports the buffer hypothesis. [2] High demands increase the risk for depression, anxiety and exhaustion irrespective of other aspects of the work environment. In order to prevent common mental disorders at work it is necessary to reduce work pace, workload, the emotional and cognitive demands, but that may be an uncomfortable fact for employers struggling to save resources and reach productivity goals.
So we know that there are risks for mental illness within the work environment. But surely we can learn how to ‘deal’ with mental illness such as depression, anxiety and exhaustion, and surely it has a lot to do with private life, work-life balance and lifestyle? And does not the individual employee have a responsibility to contribute to a health promoting work environment?
Among the most common preventive interventions that Swedish employers buy from experts concern lifestyle, such as physical exercise or smoking, and occupational health organizations offer acceptance commitment therapy to employees suffering from stress in order to get the means to ‘deal with’ their mental illness, or offer to teach them how to sleep well. Common mental disorders, including reactions to severe stress such as burnout, are considered a question of the individuals’ choices: of how to think, feel and behave, and these choices are assumed to be a question of knowledge.
Studies comparing the effect of work and non-work risk factors in the development of mental illness find that demands at work are most commonly identified as the cause – although a crisis in personal life can be what elicit the response. [7] We will have different amount of energy left for difficulties outside work depending on how much effort we have to spend and how high emotional and cognitive demands we have to face at work. These differences are not individual – they are structural. Women in healthcare are not more vulnerable for exhaustion or burnout than men because they do not know how to sleep or think, feel and behave in the right way, nor because they are more engaged in their work than any other occupational group or than men or have a vulnerable personality. They are more vulnerable because of the high cognitive, emotional and quantitative demands that tend to characterize women’s work and because of the low reward they receive in return for their effort. Who will be able to survive work as well as making personal life work is not ‘individual’ but structural. Rather than changing the individual (or forcing the individual to change herself), structural changes are needed. Placing the responsibility on the individual is a comfortable myth that absolves the employer and the society of responsibility.
When mental illness and health is considered to be a matter of individuals’ knowledge and choice, preventive and promotive interventions will place the responsibility on the individuals, not the work environment, the employer or the society. Reviews conclude that interventions that only focus on the individual – cognitive behavioural therapy, relaxation techniques, physical exercise or education about stress, sleep and lifestyle – fail to yield long-term effects for symptoms of common mental disorders unless they are combined with changes in the work environment, such as increasing control or reducing demands. [8]
Changes in the Swedish sickness insurance system the past years have generally had the aim to return individuals to work as soon as possible. The idea that work is generally good for health and wellbeing resonates through social insurance systems, with consequences for the health and wellbeing of different social groups.
What I here have called ‘myths’ are simplifications of the reality. Perhaps future research will confirm that there are resources that buffer the effect of high demands on health, and that some individual factor explain the development of burnout more than the work environment do, but as it is today, the evidence clearly indicate that consideration and amelioration of work conditions is the most effective way to prevent common mental disorders. We cannot justify inaction with lack of knowledge.
* Note on illustration - The Wonderful Wonderland of Work - Outside the Wonderful Wonderland of Work is a wasteland (a lot of its resources were used for building the wonderland). Not everyone is allowed to enter – the door is locked and those without the key patiently have to wait for the call and the opportunity to enter (however short-term), and precariously balance on the line between the wonder- and the wasteland (the more money you have to hold on to – the safer the tightrope walk). On the inside, the road claim to lead away from poverty as well as from illness. Demands for productivity and efficiency, employability and loyalty spurs us ever upwards. According to the legends, demands for profit and wealth also lead to wellbeing and health, whether we climb upwards prospering, nourished and in bloom or just by producing (ethically questionable) products faster and better. Forever upwards, we are urged to continue. We may fall as our wings are burned out, but the myths about work and mental health flutter like a wishful flying unicorn around of the Wonderful Wonderland of Work, cheering us on.
The publisher is the Centre for Welfare Reform.
Myths about Work and Mental Health © Anna-Carin Fagerlind Ståhl 2020.
All Rights Reserved. No part of this paper may be reproduced in any form without permission from the publisher except for the quotation of brief passages in reviews.
health & healthcare, mental health, tax and benefits, Sweden, Article