Anna-Carin Fagerlind Ståhl explains why long-standing evidence of work and health argues for the benefits of basic income.
Author: Anna-Carin Fagerlind Ståhl
This text will utilize theories and research from work and organizational psychology in order to analyze how a basic income may affect health. The knowledge of how work affects our health and wellbeing has been accumulating for almost a century. As welfare systems to an increasing degree rely on activation and strict conditionality and means testing in exchange for benefits, the knowledge from organizational psychology is applicable also in order to analyse effects of the psychosocial environment in welfare.
The psychosocial environment is the interaction between the individual and opportunities – or resources – in the social environment. Basic income is likely to have preventive, health-promoting and motivational potentials by acting as a resource within the psychosocial work- and welfare environment. According to Hobfoll’s Conservation Of Resources theory, resources are those things that are necessary for our survival and wellbeing, for instance money, knowledge, social support and esteem. We are motivated by the accumulation of resources and threatened by the loss of them, or the lack of resource gain after resource loss. We invest our time and our efforts hoping to gain more resources. The psychosocial environment – the opportunities the individual have to gain resources in a given environment – either promotes health in terms of subjective wellbeing and motivation, or risks strain and associated illness such as depression, exhaustion/burnout or cardiovascular disease.
Individuals have different predispositions for health and wellbeing, due to the different resources that each individual hold and have access to. Resources such as financial security, helpful and supportive networks and good health status, affect for instance how sensitive we are to resource loss and how well we can gain further resources. Resources on an individual level affects whether we can say no to precarious work conditions, how well we can navigate or manipulate the labour market and the welfare system, our level of self-esteem and our ability to gain knowledge. Our individual financial resources can be used to buy relaxation and relief from demands. The different social resources we hold enable access to information and support in how to deal with demands and gain further resources. The education, knowledge and self-esteem that we have been able to accumulate throughout our lives determine our alternatives and opportunities. Whatever health-status we have affects how well we can accumulate further resources and how hard resource loss will hit us.
The labour market and most welfare systems are governed by a work ethic, according to which paid labour is an activity that is morally superior to unpaid activities, and nothing should be given for free. A universal and unconditional basic income would accordingly risk immoral idleness, as individuals would have no incentive to perform or participate in activities. There is of course nothing immoral with engaging in activities such as caring for relatives, writing a book that perhaps no one will publish, or just taking care of oneself, just because no one is willing to pay for it. Conversely, the fabrication of weapons or emission of CO2 do not become ethically right no matter how much money you receive in return. In addition, work is also almost always considered good for health and wellbeing, a claim that is used to justify the coercion of individuals into paid labour as well as the contingencies of welfare systems. This is however not much more than a very convenient and comfortable myth for anyone who will benefit from forcing others to work. The health-promoting potentials of work depend on the psychosocial environment, in work as well as in welfare.
The effects of paid employment on illness and wellbeing of employees have been thoroughly researched. It is indeed true that a job with fair work conditions may have beneficial health-effects. It is also true that unemployment today almost always is more detrimental to health than any job, no matter how bad the conditions. However, whether work is good for health and wellbeing depends on the psychosocial environment at work and the position of paid labour in our societies. Many jobs also involve risks for illness such as depression, exhaustion and cardiovascular disease, and there is nothing inherently damaging for health in choosing to not sell your time and effort to a boss, clients or customers.
A job may promote health by providing opportunities to perform, learn and develop a sense of self-efficacy, but may also pose risks for stress-related illness such as depression, exhaustion/burnout or cardiovascular disease. It depends on how the investment of resources – time, effort and loyalty – is rewarded with potentials for resource gain: esteem, security, salary, and opportunities for learning and performing. Too high emotional, cognitive or physical demands or a lack of reward for our efforts can in the terms of stress-theory be considered threats that in the long run are detrimental to health. For instance, to have a job where it is not possible to decide how to carry out work tasks or to use skills and competencies, to work in an environment without trust or support from peer or superiors, or to work under insecure conditions and without prospects and benefits increases the risk for stress-related illness. The scientific evidence is beyond doubt: high demands, a low degree of social support and decision latitude, and an imbalance between the efforts invested and the rewards received increase the risk for depression, exhaustion/burnout and cardiovascular disease. Hence, not all work is good for health and wellbeing, although some are blessed with a job with a high resource gain not only in terms of a generous and secure income. According to a study of the French working population health actually improved after retirement, contrary to the belief that work is health-promoting in itself. There was one exception: those who truly enjoyed their work experienced a deterioration in health when they retired. Such work enjoyment is possible when work offers potentials for resource gain: opportunities to make autonomous decisions, use skills and learn new ones, and to work in a social environment of trust, cooperation and respect.
The health-promoting potentials of work also depend on the psychosocial welfare environment. Work is considered health-promoting when compared to unemployment, because even bad work conditions are most often better than unemployment. For the majority, unemployment is financially as well as socially and psychologically devastating. This is not inherent in unemployment itself. For example, a Finnish study showed that individuals with insecure employment contracts reported more symptoms of depression and exhaustion and lower self-rated health than unemployed. It is likely that it is the insecurity and the effects on social and self-esteem that makes unemployment harmful.
The positive psychology research shows that skill use, in any kind of activity, promotes motivation, enjoyment, learning and increased self-efficacy, irrespective if someone pays you to utilize your skills or not. However, to be unemployed and financially dependent on income replacement benefits enable little skill use within the current psychosocial welfare environment. Hence, some work is only health-promoting compared to the detrimental effects of being unemployed within the psychosocial welfare environment.
The work ethic is central also to the design of welfare systems. Income replacement systems such as sickness benefits and unemployment insurance are aimed to buffer periods when a person is unable to work. The activities on which benefits are contingent include actively searching for and give proof of an interest in finding a job and accepting it if offered, with significant administrative discretion as to what “suitable” may mean in terms of location or skill requirements. It also includes the participation in educational activities that are supposed to increase employability but may be below competence level. Means testing include the submission of unemployed and sicklisted to strangers’ scrutinization of their financial situation and health status. In return for the resource loss of conditionality and means testing, resources in terms of income replacement benefits and rehabilitating actions may be received.
There is little research concerning the effects of the psychosocial welfare environment on health, although studies establish detrimental health effects of restrictive policies and adversarial compensation processes. Means testing means that financial benefits and rehabilitating activities is put to an end at the sign of resource accumulation in terms of financial or health-related resources and the individual is again at risks to be plunged back into poverty or illness. This has been argued to effectively keep the poor and ill in a state of poverty and illness, in the so-called disability and poverty trap.
The model below illustrates how the balance between resource loss and gain at work and in welfare affects positive as well as negative health outcomes: individual resources affect the consequences of resource loss and possibilities for resource gain, in the psychosocial welfare as well work environment. The examples given of resource gain and loss are inspired by the Effort-Reward Imbalance Model (Siegrist, 1996) and the Demand-Control-Support-Model (Karasek & Theorell, 1990).
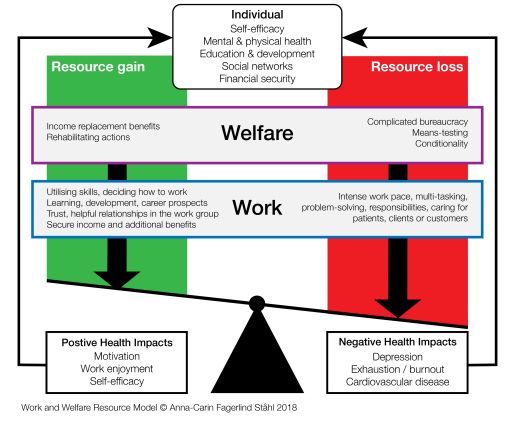
Work and Welfare Resource Model
At work, resource loss mainly concerns the investment of effort, time and loyalty in the employers’ demands for performance. Too high demands are a well-established risk for depression, exhaustion/burnout, and cardiovascular disease. This includes emotional, cognitive and physical demands. Examples of emotional demands are such as caring for patients and aiming to help people in need, or interacting with complaining customers. Cognitive demands include intense concentration, problem solving or planning, and physical demands are for example hard or intensive work with few breaks.
Resources may also be gained at work. By being able to decide how to carry out work tasks and explore new ways to work, using skills and learn new at the job we are able to gain a sense of autonomy and competence. Informational and emotional social support and respect from supervisors and peers in a trusting environment provides a sense of belonging and security. Research show that these resources promote wellbeing: motivation, work enjoyment and self-efficacy. As with high demands, low degrees of social support or decision latitude are well-established risks for depression, exhaustion/burnout and cardiovascular disease.
In welfare, the resource loss may seem lower – the activities required seldom appear very demanding and do not seem to require much effort. However, the investment of cognitive effort in the interpretation of and compliance to a complicated bureaucracy and the emotional effort to the submission to means testing must be considered from the individuals’ subjective perspective. Individuals dependent on income replacement benefits often have few resources to begin with. The substantial threat of loosing benefits makes conditionality and means testing highly demanding. Exhausted individuals, for instance, suffer from impaired working memory, attention and executive functions, cognitive functions that are necessary for the goal-directed behaviour, information processing and participation in social encounters that the welfare bureaucracy demands. The effort for someone ill is likely to be greater than for healthy individuals. To be under the threat of being refused benefits or being forced to return to a job before rehabilitated may cause substantive strain.
The opportunities for resource gain in welfare are few. Unemployed individuals dependent on benefits will be assigned activities with no opportunities to refuse or make own decisions. Those sicklisted must continuously prove their illness. Skill use and learning, even participation in social networks, are kept at a minimum due to the risk of losing benefits or rehabilitating actions as soon as work ability and health is improved. As soon as an economic buffer is accumulated, financial benefits are withdrawn.
A unconditional, universal and individual basic income would constitute a resource that reduces the negative effect of resource loss, motivates and enables further resource gain. As has been argued by others, a basic income is likely to increase employee power to refuse jobs and bargain for higher salary. With an unconditional basic income the economical, social and psychological threat and health-detrimental strain of unemployment will reduce. It will likely change the value of labour and provide an incentive for a health-promoting work environment.
No matter how much the evidence accumulates, little is done to prevent depression, exhaustion, and cardiovascular disease, or to provide the resources for wellbeing at work. There is no longer any doubt that high demands, low social support, low decision latitude and an imbalance between efforts and rewards at work is a risk. Still, organisational changes most often aim to increase efficiency by reducing “wasteful” informal social interaction and variety in how to carry out work tasks, as these activities appear to not be directly productive. This speeding up or working life and standardisation tend to reduce employee autonomy and skill use and increase demands.
There are few incentives for a reduction in work demands or increase of resources such as decision latitude and social support by merely advocating the health of employees. Employees will strive to remain at work as long as possible because the options in the labour market or as unemployed are not be better and for the most of us there will always be a group of individuals with so few resources that they have no real freedom to refuse even the hardest work environment. Employers can always find new labour to replace the shortfall created by illness or discontent, and organisational consultants who aim to promote health may at the best be able to sell it to management by highlighting the motivational and productive advantages with a health-promoting work environment.
A basic income is likely to act as an incentive for a health-promoting work environment. It will increase employee bargaining power, and not only for a higher salary. When employment no longer is the only mean for anyone without external assets to survive financially, socially and psychologically, employers will be forced to improve the psychosocial work environment in order to attract and keep employees. Resources at work both motivate and protect against stress-related illness. Health-promoting interventions today rarely target the psychosocial work environment. Instead there is a focus on behavioural and individual interventions such as mindfulness, stress-management – interventions that have a documented short term effect and is likely to mainly benefit groups of individuals with more individual level resources. A basic income will be an incentive for employers to make sure that employees have access to resources such as variety, autonomy, opportunities for learning at the job, competence development, career prospects, employment security and trust and respect from the management. The consequences will not only be motivated and loyal employees, but also a reduction in stress-related illness. In a world where employment is vital for psychological and social wellbeing and the only means for a basic financial security, a universal basic income is a key for a real improvement of a working life that is increasingly speeding up, increasingly discards individuals that cannot keep up, leaving more and more individuals behind.
The psychosocial welfare environment is today not preventive, rehabilitating or motivational, and can even be considered to be health-impairing for those who most need rehabilitation. In welfare, a basic income that is not means-tested is likely to enable a larger group of individuals to accumulate resources such as money, knowledge, health, and self-efficacy. It is likely to be directly health-promoting by enabling authority over decisions, possibilities to choose how to search for jobs, use and develop skills. In a longer run, skill utilization is likely to increase as a possible long-term effect of increased social networking and support outside work due to reduced over-employment, enabling networking with others of the same interest, building resources of skill use but also social support.
An unconditional basic income is likely to reduce the risk for stress-related illness directly, in the function of a basic resource and a means for wellbeing and survival, for gaining further resources and for enduring resource loss, at work as well in welfare. It would not only constitute a way out of the poverty and disability trap, but also be a preventive, health-promoting and motivating resource. As such, not only individuals will benefit but also organizations where employees remain in and are motivated in a more health-promoting work environment, and the society at large when resource gain rather than coercion encourage participation and performance, and enable rehabilitation of the sick.
To conclude, the health-promoting potential of work as well as welfare depends on the loss and gain of resources in the psychosocial environment. As long as individuals are dependent on paid labour, there are few incentives for employers to improve the work environment. As long as individuals are dependent on income replacement benefits, there are few opportunities for motivation as well as rehabilitation. A basic income would provide employees with power to bargain for health-promoting resources at work. From the perspective of organizational psychology and based on decades of research, a basic income would constitute a protection against stress-related illness but also the foundation for health, subjective wellbeing and motivation in work as well as welfare.
Harvey S et al (2017) Can work make you mentally ill? A systematic meta-review of work-related risk factors for common mental health problems. Occupational Environmental Medicine, 74, 301-310.
Hobfoll S (1989) Conservation of resources. A new attempt at conceptualizing stress. American psychologist, 44, 513-524.
Virtanen M, Kivimäki M, Joensuu M, Virtanen P, Elovaino M & Vahtera J (2005) Temporary employment and health: a review. International Journal of Epidemiology, 34, 610-622.
Westerlund H et al (2009) Self-rated health before and after retirement in France (GAZEL): a cohort study. The Lancet, 373, 1889-1896.
Lippel K (2012) Preserving workers' dignity in workers' compensation systems: an international perspective. American Journal of Industrial Medicine, 55, 519–536.
Barr B, Taylor-Robinson D, Stuckler D et al (2015) Fit-for-work or fit-for-unemployment? Does the reassessment of disability benefit claimants using a tougher work capability assess- ment help people into work? Journal of Epidemiology and Community Health, 70, 452–458.
The publisher is the Centre for Welfare Reform.
Basic Income is Good for Your Health © Anna-Carin Fagerlind Ståhl 2018.
All Rights Reserved. No part of this paper may be reproduced in any form without permission from the publisher except for the quotation of brief passages in reviews.
Basic Income, health & healthcare, nature & economics, tax and benefits, Europe, Article