This essay argues that the integration of social care and healthcare funding in Mental Health is still a priority and highly feasible.
Authors: Simon Duffy, Clare Hyde, Carole Green and Steve Stericker
In 2010 mental health leaders in Yorkshire & Humber backed a statement describing the desired future for mental health services called Personalisation in Mental Health.
This statement included a number of goals:
There remained several technical challenges to overcome in particular there was great interest in exploring whether it was possible to build an integrated Resource Allocation System (RAS) for Mental Health services. To test this possibility a pilot was begun in Kirklees. However, after a short period leaders in Kirklees determined that they could not go ahead with this process.
This report has been drawn up by the regional Personalisation Steering Group for Mental Health to reflect on the lessons learned.
There are only a very small number of people who have taken any technical interest in both the development of Payment by Results (PbR) in mental health and the development of Resource Allocation Systems (RAS) for personalisation. Hence it is not surprising that there is tremendous room for confusion. These technical innovations are not doing exactly the same work - however the two technologies can be combined.
Payment by Results in mental health depends upon being able to establish:
Before the advent of personalisation such a methodology was primarily focused on enabling commissioners and providers within the NHS to have better conversations about:
This approach has now been made mandatory by national policy and it seems to be a useful and powerful way of moving conversations about funding in a progressive direction towards outcomes, innovation and community development and away from purely service-defined institutional solutions.
However this approach could also benefit the drive towards personalisation. A tariff is not an individual budget.The precise figure that an individual will need to achieve recovery will not be identical to the average cost for that cluster.
There are other factors that will effect cost and which within the PbR system will be averaged out within the tariff:
However this does not get in the way of building a cluster-based RAS - quite the opposite. Precisely because the cluster (which is always identified) can be tallied with an average figure (which will be reasonably robust) it will be straightforward to define a stepped RAS that practitioners and individuals can use to calculate an individual budget and begin developing more personalised and effective solutions (see Figure 1).
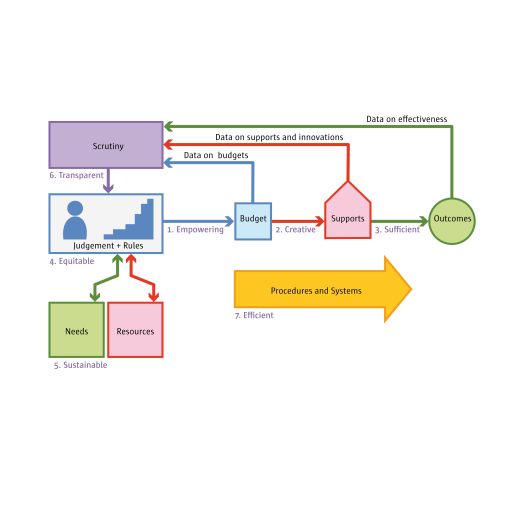
Figure 1. Stepped RAS Based Upon Tariff Average
This kind of approach is also in harmony with a growing desire amongst practitioners to treat the RAS more as a tool to encourage good practice and to avoid undue bureaucracy and complexity in the calculation of individual budgets (see Simplify the RAS).
So, to summarise, the Mental Health PbR currency model is a natural starting point for calculating an individual budget. It simply needs practitioners to also be equipped with a suitable simple system for working with and around that average figure and safeguarding overall spend. This can be done using a very simple methodology.
The initial intention in Kirklees was to pilot individual budgets for people using the Assertive Outreach Team (AOT). As no piloting was actually carried out it is impossible to be sure that it would have been successful, but what was striking from conversations with AOT members was that personalisation seemed to have the potential to bring enormous benefits to their work.
For example:
Team members expressed a strong desire to work in a more flexible and person-centred way but the current system of care management would require changes to facilitate such a personalised approach as is currently underway in adult social care (see Figure 2).
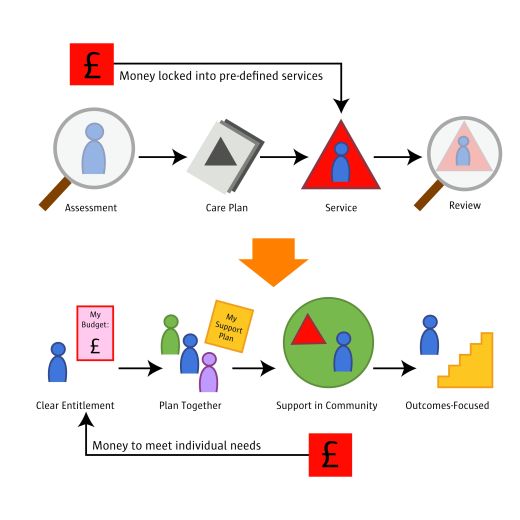
Figure 2. The Shift to Individual Budgets
In adult social care progress towards personalisation hinged critically upon the willingness of social workers to rethink their role. As the social worker saw their role shift towards a co-producer, with the individual, of better outcomes and more creative solutions then the system as a whole began to shift.
This change involves professionals and organisations moving beyond worn-out models of ‘purchasing’ and ‘providing’. Providers themselves can be the agents of change - developing more personalised supports solutions with people and helping people to make better use of community. Limited conceptions of service providers - defined only by some existing pattern of service delivery turn out to be self-defeating.
To date there has been limited success in achieving the real benefits offered by pursuing personalisation. Further progress may well depend upon the willingness and understanding of existing NHS service commissioners and providers to shift their role in a number of respects.
For example:
Moreover, the currency system could even be used to incentivise the shift to recovery (although there are always risks in using funding systems in this way) because a service provider would benefit from helping people become less dependent upon services if they were funded by the final outcome not the on-going service. Moreover, the national approach to commissioning services on the basis of outcomes is a growing trend across a range of areas.
However a fear of many observers of the mental health scene is that we are not moving towards a model where NHS service providers have embraced personalisation. A climate of mistrust between commissioners and providers can also encourage the fear that service providers will exploit the emerging model only to increase their own funding at the expense of community options and higher quality solutions, or that commissioners will use this to reduce expenditure on mental health services.
To state this fear however simply underlines the choice ahead of us. It is quite possible for NHS service providers and commissioners to play a leading role. Moreover it could be argued that until they actually play this role then mental health services will be frozen into unnecessarily inflexible and institutional solutions. Only those responsible for commissioning and providing mental health services can make this change and this is a matter of their leadership and their vision.
Arguably local authorities should be particularly keen to help their NHS colleagues make this shift in role in support of better commissioning and better practice at every level.
The most fundamental barrier to integration appears to be a lack of trust. Agencies cannot pool resources unless they can believe that joint working will lead to mutual and enhanced benefits.
However there are very good reasons to integrate:
However the barriers to integration remain and some of these are set out in the report from Kirklees describing their reasons for terminating the project:
This last point demonstrates the central challenge – how to enhance recovery and reduce dependence and use of high cost intensive services and thus facilitating a move in investment from secondary care to primary and preventative approaches. If managed well individual budgets could create exactly the right conditions for this type of change to occur.
The above barriers, and others, were experienced as very real and tangible challenges to the Kirklees project. Despite the challenges, it is the view of steering group that there are already models of integrated practice across the UK and national policy is to promote such models. Hence, it seems that workable solutions could be found for the benefit of people who access mental health and community services.
In our view the achievement of greater integration will demand:
The key to success will be for mental health service providers and commissioners to start working with people who access services in a more personalised way. This will require everyone concerned to embrace personalisation in a robust way.
The good news is that the mental health PbR currency model can help this process. But this will still require continued leadership and commitment in a challenging environment that often throws up disincentives to more integrated approaches. This can then perhaps be the way in which greater integration might begin.
The publisher is The Centre for Welfare Reform.
Integrating Mental Health Funding © Simon Duffy, Clare Hyde, Carole Greene and Steve Stericker 2011.
All Rights Reserved. No part of this paper may be reproduced in any form without permission from the publisher except for the quotation of brief passages in reviews.
health & healthcare, local government, mental health, Resource Allocation Systems, Article