An example of how UK primary care can offer safer more supportive personalised care whilst saving money at the same time.
Author: Dr Brian Fisher
Here is an example of how UK primary care can offer safer more supportive, personalised care while saving money at the same time. In essence, this evidence-based process offers people with long-term conditions such as heart disease and diabetes regular follow-up and review by telephone. The call asks how the person is getting on but also encourages people to feel more confident about looking after themselves better. To maximize the beneficial effect, the aim is to link this process with “reablement” through social care and befriending through the voluntary sector.
The paper is based on a proposal for reform in Lewisham and goes on to outline the practical changes it would require in local systems.
Ed Wagner writes the following:
A colleague with rheumatoid arthritis likens the experience of living with chronic illness to flying a small plane. If it is flown well, one gets where one wants to go with the exhilaration of mastering a complicated set of challenges. If it is flown badly, one either crashes or lands shakily in the wrong airport, reluctant to ever leave the ground again. The patient must be the pilot, because the other possible pilot, the health care professional, is only in the plane a few hours every year, and this plane rarely touches ground.
If chronically ill patients must pilot their planes, then the role of health care is to ensure skilled pilots, safe planes, flight plans that safely get the pilots to their destinations, and air traffic control surveillance to prevent mishaps and keep them on course.
Medical care then must assure that:
Evidence suggests that the typical acute problem–oriented visit is a barrier to such care.
Implementation of this holistic approach, called the chronic care model (CCM) in the US, has been shown to improve outcomes in diabetes, depression, and congestive heart failure. Interventions that included at least 2 CCM components reduced risks for emergency/unscheduled visits and reduced length of stay in hospital
Interactions are more likely to be productive if patients are active, informed participants in their care. Patients must have the information, skills, and confidence to make best use of their involvement with their practice team.
Such interventions appear to cluster in these areas:
Effective self-management support and links to patient-oriented community resources help to activate and inform patients and families to better cope with the challenges of living with and treating chronic illness.
Traditional patient education emphasized knowledge acquisition and didactic counselling. However, mounting evidence indicates that while such interventions increase knowledge, they are unsuccessful in changing behaviour or improving disease control and other outcomes.
Instead, more recent theoretical and empirical research has shifted the focus to:
Self-management demonstrations and role-playing in learning sessions to help communicate the differences seems to offer the best outcomes.
To enable practice teams to have productive patient interactions, the organization must assure that the teams have the expertise to provide appropriate clinical and behavioural management.
The effective control of most chronic diseases requires appropriate medical therapy as well as competent self-management. Guidelines or protocols are useful starting points. But effectiveness studies consistently show that introducing guidelines has only a minimal impact on quality unless guidelines are integrated into the practice through education, reminders, specialist involvement, or other decision-support interventions.
Practice teams must have the necessary expertise, relevant patient information, time, and resources to act, rather than just react, to ensure effective clinical and behavioural management.
High-quality chronic illness care requires primary care to consistently provide the assessments, support for self-management, optimization of therapy, and follow-up associated with good outcomes. These interactions do not necessarily require face-to-face visits. Ample evidence documents the effectiveness of using the computer or telephone for this purpose.
Most practices in the UK have standardized or organized approaches to collecting, summarizing, and reviewing individual or aggregate patient data to facilitate care. Effective programs assure access to timely, relevant data about individual patients and populations of patients from clinical information systems. A computerized disease registry that includes critical information about each patient and the performance and results of important aspects of care enables care teams to call in patients with specific needs, deliver planned care, receive feedback, and implement reminder systems.
Effective chronic illness management calls for a delivery system design that encourages and enables productive interactions. The multiple tasks involved are more likely to be accomplished with the delegation of care from the physician to others on the team. Several studies have demonstrated the added benefits of ready access to nurse case managers and other professionals who have the skills and time needed for optimal self-management support and assistance with disease control. Chronic disease management also benefits from innovations in the scheduling and organization of visits.
The longer time horizon and fluctuating course of many chronic illnesses requires regular interaction between caregivers and patients. The Institute of Medicine report described this as a "continuous healing relationship" and argued for the increased use of methods of interaction other than face-to-face visits. The use of the telephone, for example, allows for more intensive, yet cost-efficient, follow-up of chronically ill patients and has been associated with improved outcomes in a variety of chronic diseases.
In Lewisham we have a number of elements already in place. These include:
However, in order to deliver this systematically, restructuring is required both for practices, community services and Social Care and Health. In the current situation in Lewisham, it may be possible to commission some of the service from University Hospital Lewisham who run our community services.
Closely linked to GP surgeries or commissioning clusters, the aim of the role would be to monitor elderly patients registered at every practice by providing regular consultations either at the GP practice or in their own home. This would provide reassurance and support for patients whilst providing an early warning for those patients with deteriorating health. A key part of this role should aim to increase confidence and self reliance by promoting self care techniques and give health promotion advice (e.g. healthy eating, exercise advice) In addition provide links to local organisations and support groups to help those patients who may be isolated and live alone.
This service could be commissioned by Lewisham PCT or by local Practice Based Commissioning groups. Croydon PCT currently have a number of specialist Health Visitors who provide this service. In Lewisham a Practice Nurse at Sydenham Green Health Centre runs a successful service.
Activities to underpin a more effective model for long-term conditions (LTCs) would therefore include:
If this scheme were linked with Social Care and Health, then a number of important activities could also be commissioned:
If this scheme were linked with community groups and community development, then even more benefits would accrue:
If everyone with a Long Term condition had direct access to their own medical records then this would also improve compliance and self-help - the technology exists to make this possible.
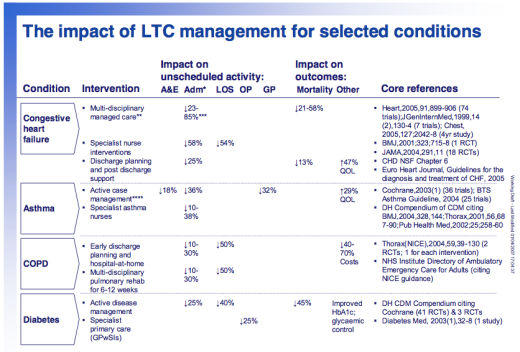
[Image taken from the Report of the Long-Term Conditions Clinical Working Group]
The publisher is The Centre for Welfare Reform.
Proactive Primary Care © Brian Fisher 2011.
All Rights Reserved. No part of this paper may be reproduced in any form without permission from the publisher except for the quotation of brief passages in reviews.