Personal Budgets do not need to reinforce individualistic consumerism, they can be a route to a more collective approach where care is shared.
Author: Thomas Allan
“Organisational form is fundamental to the relationship between the content of social care and the systems that provide it”
Restakis, 2011
Over recent decades, forces for change in social care for adults with a learning disability have gathered around widespread discontent about older systems of paternalistic care. The provision of support through fixed, inflexible rotas that revolve around time and task, rather than relationships, choice and positive life affirming outcomes is a classic example. Addressing this has been the goal of the Personalisation movement in the UK: the drive for care and support services that are tailored to the needs of individuals, rather than designed and delivered in one-size-fits-all systems.
Yet today, in the 21st century – and despite a raft of market-driven change and technological innovation – our social care system still widely fails to respond to the needs or build upon the assets of marginalised citizens and communities. The inflexibility of care provided through regimented state-systems is well known. But it is too simplistic to say we are only battling the institutionalized practices of the past.
Personalisation has often been narrowly conceived of in terms of the funding of social care, such as Personal Budgets. This has had the effect of limiting its’ potential benefits by individualising funding methods to socially isolated citizens, or as an efficiency framework for local authorities.
Moreover, it is often argued that one of the main barriers to providing more personalised social care services is that demand for social care outstrips the resources the government is making available. The challenge is not only one of funding, but the ways in which social care is conceived of, organised, and provided. In short, Personal Budgets needs a partner project: the creation, experimentation, and provision of social care through distributed systems and accountable, human-scale alternatives.
If the current pandemic is teaching us many important lessons, one of the most urgent is that generating more responsive forms of support for all citizens who need it is not just a preferred future, but a here-and-now social reality. Any post pandemic era must be characterised by meaningful, resilient, and sustainable systems change, rather than a return to the fragility, injustices, and short-termism of ‘business-as-usual’.
“A Personal Budget is an agreed amount of money that is allocated to you personally by your local council (and other funding streams) following an assessment of your care and support needs. This is support that you decide and control, in other words you control the money for your care and support. It allows you (or your representative) to control the financial resources for your support and the way the support is provided to you.”
Disability Rights UK
Personal Budgets were seen by policy makers and local authority commissioners as a means of putting the philosophy of personalisation into place in frontline care and support services. The intention was to give control over resources to the citizen who needed them, rather than providing them with services in a restrictive, paternal manner. Personal Budgets can be managed in three main and contrasting ways:
A commissioned budget
The local authority will choose a support provider, pay the provider direct who will receive the funds and provide direct support according to local authority instructions, albeit in line with the persons wishes as far as practicable. One of the main criticisms of this arrangement is the lack of control it affords the person receiving support, as well as a demonstrable inflexibility to their experiences, nuances, and choices. In addition, commissioned budgets are also a recipe for low accountability, as Next Systems advocate and academic John Restakis (2011) explains:
“[when] service organisations retained full control of the funds…the users of these services had little or no role in influencing the content or the quality of the care they received…nor was it easy…to seek more appropriate care elsewhere if they were unhappy. The funded groups were established organisations, secure in their funding, and had little incentive to change so long as power remained exclusively in their hands. Accountability flowed to the funders, not to the people they were meant to serve…Under third party contracts, the buyer [the local authority] does not consume the services acquired, the [person supported] does not pay for the services received, and the [service provider] stands in the highly advantageous position of dealing with a buyer who rarely sees what is purchased and a consumer who never bears the expense.”
Direct Payments
These are funds given directly to citizens to organise and pay for support arrangements themselves. The introduction of Direct Payments marked a shift from funding the supply of social care (paying the organisation to provide the support) to funding its’ demand (paying the person direct). By giving the funds to citizens they assessed as eligible to receive them, local authorities would break the pattern of individuals and families locked into unhappy commissioned support arrangements through the introduction of a simple, two-way relationship.
But Direct Payments are also an arrangement where people who qualify for support can be required to take on the role and responsibility of purchaser or direct employer of their own workforce (Catley & Duffy, 2018). This means – and as Restakis (2020) again points out – Direct Payments often leave citizens isolated and vulnerable without the resources or support for managing the complexities of certain care provisions that require:
Individual Service Fund (ISF)
Alternatively, an Individual Service Fund (ISF) can be offered as a midpoint to the above two methods. An ISF arrangement looks something like this:
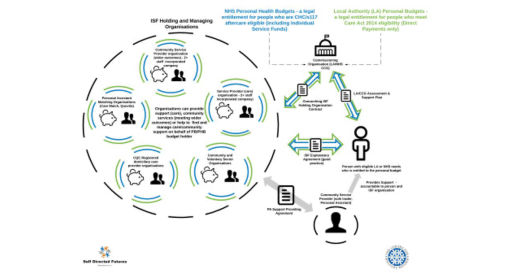
While ISFs are similar in principle to a Direct Payment (in terms of aiming to offer choice and flexibility), the funds can be held by a trusted support provider of the person’s choice. In theory, this can allow for creative and supported use of budgets. For example, using funds flexibly as the need arises, or to pay for a Personal Fitness Instructor. The idea is that it allows for different sorts of relationships to flourish beyond the limitations of the supporter-supported binary, reflecting the flux and transient nature of everyday community lives.
“An ISF is an internal system of accounting within a service provider that makes the personal budget transparent to the individual or family. This helps provide flexible support by making the organisation accountable to the person.”
Think Local Act Personal, 2015
But does it? For proponents of ISFs, they are effectively a midpoint between a Direct Payment and a directly commissioned service (Watson, 2019). However, the role of support providers themselves as holding organisations raises a question. Some revised practices of budget transparency aside, to what extent do ISFs really differ from a commissioned budget? (Watson, 2020a).
One benefit of choosing an ISF is that they offer an alternative route for people who do not wish to take on the responsibility of a Direct Payment. However, without an independent agency or community broker assisting people in the identification, evaluation and contracting of care services (or more intriguingly, owner-control rights in the holding organisations), people who need support are still potentially vulnerable to the restrictions of third party contracting (e.g. the self-interest of support providers), with limited control to influence the direction of their support.
Situated in the right supportive context, ISFs enable people to create their own life pathways, with added opportunity to co-produce efficient, effective support, whilst maximising local resources. How might we maximise the opportunities afforded us by Personal Budgets (and the topical nature of ISFs) to develop more accountable, locally responsive, and human scale provision of social care? We refer to three organisational forms that help point us in the right direction.
Micro-Enterprise
“Micro-enterprises (also called micro-providers) are very small organisations delivering social care services that employ five or fewer staff (full time equivalent). They are usually independent of any larger organisation and are offered by a range of people and organisations in the community, including people who are disabled or need support themselves.”
Needham, Allen & Hall, 2015
Micro-enterprises are driven by community spirit, creativity, and a desire to do things differently. But to date they have been primarily reliant upon the flexibility of self-funding or Direct Payments, and are still relatively small-scale providing only limited capacity in comparison to other more developed sectors of the market (Needham, Allen & Hall, 2015; Watson, 2020b). With one key barrier for micro-enterprises being low uptake of Direct Payments (Needham, Allen & Hall, 2015), and a personal budget managed by the local authority (commissioned budget) still unlikely to be able to be used to pay for support from a micro-enterprise, flexible funding methods such as ISFs could represent one possible route for their multiplication.
A report based on an evaluation of micro-providers in England by the University of Birmingham in 2015 found that:
“…micro-enterprises deliver more personalised, innovative and valued support for a similar or lower cost than larger providers. These benefits seem to be based on the micro-enterprises having greater continuity of staff, greater staff autonomy and greater accessibility of managers compared to larger organisations.”
Needham, 2015
Additional outcomes of the report found that micro-providers were able to:
However, micro-enterprises and other small community-based providers face formidable challenges convincing public authorities they can be trusted with public welfare at the level of scale (moving beyond niche provision or experimentation) (Conaty, 2014). How can they harness the resources required to survive, develop, and multiply? More controversially, how can they convince public authorities to prioritise smaller-scale alternatives? Despite the evidence, commissioners and policy makers maintain a tenacious fixation on the false economics of economic ‘efficiency’, continuing to subsidise large scale, often debt loaded providers only able to offer poor quality and distant ‘care’ through steep vertical chains of command.
Despite these challenges, Infrastructure light micro-enterprises based on nimble, non-hierarchical and peer-to-peer relational dynamics can operate on a scale better suited to connecting with local people and communities. Such models of support have the autonomy, continuity and accessibility built into their operations that can catalyse creativity and solutions in real time. This is essential to address the shifting barriers and exclusions marginalised citizens and communities face.
Buurtzorg Neighbourhood Teams
Buurtzorg is a not-for-profit social enterprise and managerless network of District Nurses providing home care in the Netherlands since 2006. Through autonomous support assembled around the assets of citizens, families, neighbourhoods, and communities, Buurtzorg is demonstrating a capacity to connect with multiple stakeholders in a much more responsive, cost effective and flexible manner.
Catalysed by the frustration and innovative thinking of Jos De Blok, Buurtzorg mark a shift away from the declining quality, rising costs, and fragmentation associated with privatised and centralised models of home care. Their aim is to separate the provision of care from the administrative process – ‘humanity over bureaucracy’ – making traditional management and bureaucracy surplus to requirements:
“...a shift from predicting, specifying, commissioning, modelling, building, measuring, planning, managing, auditing, and reporting on services (incidentally, jobs with lower job satisfaction) to serving on the frontline (higher satisfaction)”.
Thompson, 2015
To assist with this, Buurtzorg utilise a digital platform that facilitates peer-to-peer collaboration: Buurtzorgweb. This enables the distributed living cells of the system (Neighbourhood Teams) to connect to one another; share relevant information such as practice or financial data; create space for discussion, innovation and the sharing of new ideas; and engage with external quality inspectors and funders, among other things (Murray, 2015).
Buurtzorg thus becomes a distributed network that puts the citizen – not the support provider or commissioner – at the centre of support. In this model, a wide range of stakeholders are trusted, treated as equal peers, and considered of equal value as part of a transparent process of designing and providing care. This is as opposed to a state-controlled or consumer, for-profit model of care, where the potential for dignity and autonomy (let alone co-production) is limited, or where people are reduced to passive consumers in a supply chain (Pestoff, 2012). In contrast, Buurtzorg is a participatory model; a new production matrix generating holistic care.
Buurtzorg, however, face equally formidable challenges. Transitioning from a model with relatively valued health care staff with professional qualifications (i.e. District Nursing) to low paid and undervalued social care staff is one. In this sense, how might Buurtzorg address the tensions between the devalued labour of care (the low wages, emotional exhaustion and poor working conditions that is characteristic of much marketized care provision in the UK) and the drive for more flexible, personalised care? How are Buurtzorg navigating the transition from mainly insurance funded (90%) care in the Netherlands to the dominant state commissioned funding in the UK? Finally, could self-ownership enhance the self-management model of Buurtzorg?
Multi-stakeholdership and Multi-stakeholder cooperatives
Multi-stakeholder governance reflects and supports a given citizen or community’s self-defined needs. Through multi-stakeholdership we see examples of what can be achieved when support workers and carers, owners, families, volunteers, and community supporters work in partnership with public authorities on a much more transparent and reciprocally empowered (non-hierarchical) basis. As P2P Foundation founder Michel Bauwens explains:
“Key here is that care services are funded as a public service by the state, guaranteeing universal access, but the crafting of the process is a co-production of all stakeholders, including [citizen] communities and their families. [Citizens] have a quite different vision of what they need than process oriented [services], resulting in soaring satisfaction rates… Multi-stakeholdership and the co-production of the value chain includes everyone affected by a provisioning service.”
Bauwens, 2014
Multi-stakeholder cooperatives are social and solidarity economy enterprises with democratic and multi-stakeholder representation in their decision-making structures. There are several benefits to this approach as demonstrated by the example set in Bologna, Italy, which now accounts for 87% of all social services contracts in the city (Mendell & Restakis, 2014):
Multi-stakeholder cooperatives have emerged in Italy and elsewhere as a practical response to address the inadequate provision (and unequal distribution) of both state and commercial market based social care services. As such, they represent a unique opportunity for change. However, Cooperatives UK note a number of obstacles to their development and growth in the UK, including a lack of understanding of their form and function, policy prejudice, and ‘a lack of practical experimentation with a generative new frontier that other countries are demonstrating’ (Conaty, 2014).
Despite their differences, what is apparent in the above examples is the critical importance of the relational nature of care. All three have an operational focus on the exchange of human relations and aim to generate (or make more visible) forms of social value in the provision of good quality and effective care. In coming to our recommendations, we note however many personal, inter-personal and organisational factors need to converge to create the right synergy for success.
These include:
This itself represents a formidable challenge and a narrow margin for error, especially in our current pandemic, as well as recent economic outlook and policy culture (i.e. austerity). However, we would recommend the following as ten starting points for change:
1. The continued use and increased uptake of Direct Payments and ISFs, but alongside an increase in the capacity of independent, civil society organisations (i.e. consumer cooperatives) acting where appropriate as:
These civil institutions could also act as community support brokers in the identification, evaluation, and contracting of care services, as well as offering conflict resolution or mediation. Support providers who qualify for receipt of ISFs should confer control rights over the design and delivery of support in their operations (Restakis, 2011).
2. Prioritisation in policy for Social Economy organisations for the use and implementation of Personal Budgets. Many social economy organisations – cooperatives, community owned trusts, community interest companies, social enterprise, small charitable organizations – are already orientated towards the common good and community resiliency. These organisations grow as solutions to the failures of either state provided or market-driven care provision, and are often more closely attuned of the views, assets, experiences and needs of people who need support.
3. The establishment of social markets (Restakis, 2017). Social markets operate for non-commercial purposes (surplus value or profit that is orientated towards the social benefit of people and communities); provide the institutional foundations for the flourishing of human relations; and support social economy organisations to gain skills and resources. Examples of social markets are those operated through social currencies or reciprocity-based time banking systems. However, the development (and public support) of social markets can help facilitate forms of social financing (e.g. credit unions) that help smaller, civic organisations with a social purpose gain access to capital, reducing their dependency on the state or capital markets.
4. The experimentation with multi-stakeholder cooperatives. Multi-stakeholder cooperatives could be the most effective and accountable form of care provision since they expand their operations to include the interests of the wider community as well as their members. They have also demonstrated a capacity to work innovatively and transparently in partnership with local authorities (see Restakis, 2011; 2017; Mendell & Restakis, 2014).
5. The exploration of alternative, social accounting methods that go beyond a sole focus on financial performance indicators. These methods, often utilised by social economy organisations, can include strategies for improving human wellbeing and establishing legitimacy at a community level. Properly designed and implemented, social accounting can make the social benefits of care more visible and adaptable to people who need support (members) and other key stakeholders in society (Jayasinghe & Thomas, 2014).
6. Experimentation with the pooling of Personal Budgets supported by community brokerage and enacted through Neighbourhood Democracy.
7. The growth of socio-legal partnerships to address the growing deficit in control for citizens in real terms.1 This is necessary to offset or reverse the recent policy tendency of national governments to download their obligations onto lower levels of governance (e.g. ‘Big Society’ narratives), but without providing a proportionate level of legal authority or funding support (Bollier & Weston, 2013). Citizens must have the resources to insist on a more personalised ‘Partner State’ that maintains its’ commitment to the funding and community level provisioning of social care services, without resorting to controlling or dominating its’ generation or operations.
8. The expanded use of peer-to-peer IT networks (both within and between organisations) can help to foster distributed governance and citizen involvement; to enable the digital infrastructure for peer-to-peer collaboration and the free exchange of ideas and feedback in the design and experience of support services; as well as the open sharing of relevant information between partners (see Restakis, 2017).
9. Recognition among policy makers, support providers and commissioners alike that the changes required are essentially qualitative. Much will depend on whether we can shift our outlook from evaluating social care based on outdated industrial modes of thought to a new paradigm that more closely reflects its’ true nature and characteristics (Allan, 2016). This will include, for example, the development of ecological, participatory design and evaluation principles that reject centralization and instead promote resilience and durability through distributed systems. Ultimately, the management of care as an inalienable human right, and as a protected commons (managed by a cooperative community of users, according to their own rules and norms) situates Personalisation and indeed social care within a broader spectrum of social value and rights.
10. Finally, the establishment of (preferably publicly funded) regional communities of practice to act as systems leaders on behalf of the social economy. The purpose of such roles would be to combine advocacy, innovation, and coalition building locally and globally to catalyse collective action in support of change at a systems level (much as Citizen Network is currently doing). The goal is to ensure the development of locally responsive social care services accountable to citizens and communities.
Personal Budgets and the Personalisation movement should be understood within an expanded vision of social care and holistic systems change. Personalisation is more than just a statement or policy of intent, a target for compliance, or a change in individual behaviour or practice. It is time to develop a more compelling paradigm to situate innovation and change in social care within a wider framework for transition to a just, sustainable, and more caring economy.
Note:
1. The Centre for Adult Social Care – Advice, Information and Dispute Resolution (CASCAIDr) is a registered charity currently doing a remarkable job operating in a no-mans-land between market and state on no state funding, and acting as a proxy for what some might argue state forms themselves should be doing. That is, upholding adults health and social care rights through access to knowledge, information and helping people fulfil their legal right to care and support services.
References
Allan T (2016) Beyond Efficiency: Care and the Commons. Centre for Welfare Reform
Bauwens M (2014) Michel Bauwens on the rise of multi-stakeholder cooperatives. https://www.shareable.net/michel-bauwens-on-the-rise-of-multi-stakeholder-cooperatives/
CASCAIDr (The Centre for Adult Social Care – Advice, Information and Dispute Resolution) https://www.cascaidr.org.uk/
Catley A & Duffy S (2018) Beyond Direct Payments: Making the case for micro-enterprise, Individual Service Funds and new forms of commissioning in health and social care. Think Local Act Personal.
Conaty P (2014) Social Cooperatives: A Democratic Co-production Agenda for Care Services in the UK. Cooperatives UK https://www.uk.coop/resources/social-co-operatives-democratic-co-production-agenda-care-services-uk
Disability Rights UK Personal Budgets: The Right Social Care Support Disability Rights UK Fact Sheet F72 https://www.disabilityrightsuk.org/personal-budgetsthe-right-social-care-support
Jayasinghe K & Thomas D (2014) Alternative and social accounting (Chapter 18) in The Routledge Companion to Alternative Organisation eds. Parker, Cheney et al. Routledge
Mendell M & Restakis J (2014) Public Policy for a Social Economy. Flok Society https://floksociety.org/docs/Ingles/3/3.2.pdf
Murray R (2015) Notes for Social Care Forum dialogue October 16th, 2015. Unpublished report
Needham C (2015) Do micro enterprises offer care and support on a scale that’s just right? https://socialcare.blog.gov.uk/2015/06/30/do-micro-enterprises-offer-care-and-support-on-a-scale-thats-just-right/
Needham C, Allen K & Hall K (2015) Micro-Enterprises: Small enough to care? University of Birmingham
Pestoff V (2012) Innovations in Public Services: Co-Production and New Public Governance in Europe (Chapter 2) in Towards Peer Production in Public Services: Cases from Finland eds. Botero, Paterson et al. Aalto University Press
Restakis J (2011) Humanizing the Economy: Cooperatives in the Age of Capital. New Society Publishers
Restakis J (2017) Cooperative Commonwealth & The Partner State The Next System Project https://thenextsystem.org/cooperative-commonwealth-partner-state
Restakis J (2020) Private correspondence dated 15th May 2020
Think Local Act Personal (2015) Individual Service Funds (ISFs) and Contracting for Flexible Support https://www.centreforwelfarereform.org/uploads/attachment/529/individual-service-funds-isfs-and-contracting-for-flexible-support.pdf
Thompson M (2015) UK voters are being sold a lie. There is no need to cut public services. The Guardian https://www.theguardian.com/public-leaders-network/2015/feb/12/uk-voters-cut-public-services-amazon-spotify-uber
Watson C (2019) A Commissioners Guide to Individual Service Funds. Centre for Welfare Reform
Watson C (2020a) The Legal Framework for Individual Service Funds. Centre for Welfare Reform
Watson C (2020b) Meeting urgent demand with new models of care and Individual Service Funds. Institute of Public Care
The publisher is the Centre for Welfare Reform.
Putting Personal Budgets in Their Place © Thomas Allan 2020.
All Rights Reserved. No part of this paper may be reproduced in any form without permission from the publisher except for the quotation of brief passages in reviews.