Cat Wood faces multiple challenges within the mental health system but peer support is helping.
Author: Cat Wood
Cat Wood shared her experiences of mental health systems at a Mentally Well Alliance meeting in Doncaster in April 2025. This is the transcript of her talk.
Thank you for inviting me to the Mentally Well Alliance meeting, I’ve come to share my experience of having autism.
I was diagnosed with autism on the 19th September 2019, that date is also memorable to me as 5 years prior, in 2014 , was the first date I was admitted as an inpatient in RDaSh Doncaster St Cath’s,. I’ve been an inpatient twice, the second time was in 2015.
I’ve had 8 years in the mental health service without an autism diagnosis. In those years my hospital stays were not a good experience
One criticism I’ve found with the mental health service, and across the board and with the health service, to be honest is communication and explaining things. I, like a lot of autistic people, am a logical thinker. I’m not good at maths, but if you give me something that doesn’t add up, I’ll want an explanation, and it will ruminate if you don’t. However, many of the mental health service thinks it can be something I can just get over, or one CPN just told me to “accept being unhappy.”
But I find it rare to come across a professional who accepts me for who I am and is patient enough for me to actually think of what I want to say or even do things like audiology and visual field tests, I have co-ordination issues with my autism so explaining I require a warm up round on those tests isn’t sometimes accepted.
I’ve grown up in hospital - Sheffield Children’s Hospital, Rygate Children's Centre and in and out of A&E and since the diagnosis – some professionals do things to you, treat you like a child, they talk at you, or to the other adult in the room, leaving you more frustrated.
This leads to other forms of communication, understanding body language and eye contact. It was actually how it was noticed I could have autism; I am horrible at making eye contact. Like many late-diagnosed females, I was just dismissed as being shy when younger, and the MH service gave me a diagnosis of EUPD before this. I had an experience with a GP despite also being in a depressive cycle, with having a mood disorder, cyclothymia, I was forced to make eye contact and sit up straight despite defending myself, stating I have autism. But to them, I had a “trust issue.” I ended up in A&E a few days after this, attempting to overdose.
As someone who’s late diagnosed, it's horrible to have the condition invalidated, after being bullied and struggling for so long masking, pretending to be someone who fits into the “norm” which is often tiring – think about trying to calculate everyone’s next move so you know what to do or say next so you hope you don’t look like an idiot to them, being told to “not let it define you,” when all you do is fight against society to get them to accept and make adaptions for how your brain is wired so it’s less stress on you.
Autism is something all health professionals should accept, as I know it affects me and a lot of people in so many ways. And that sort of attitude is harmful.
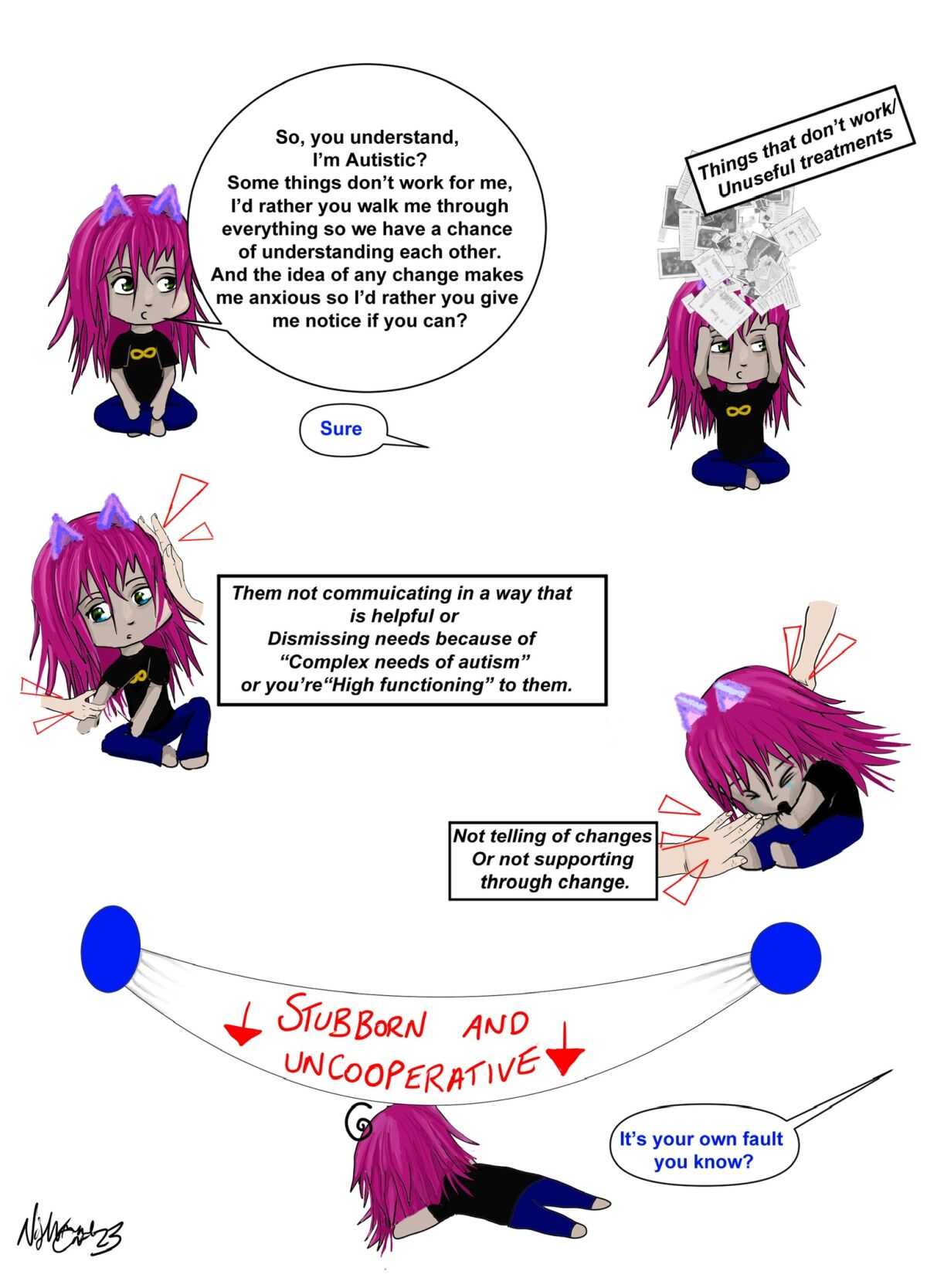
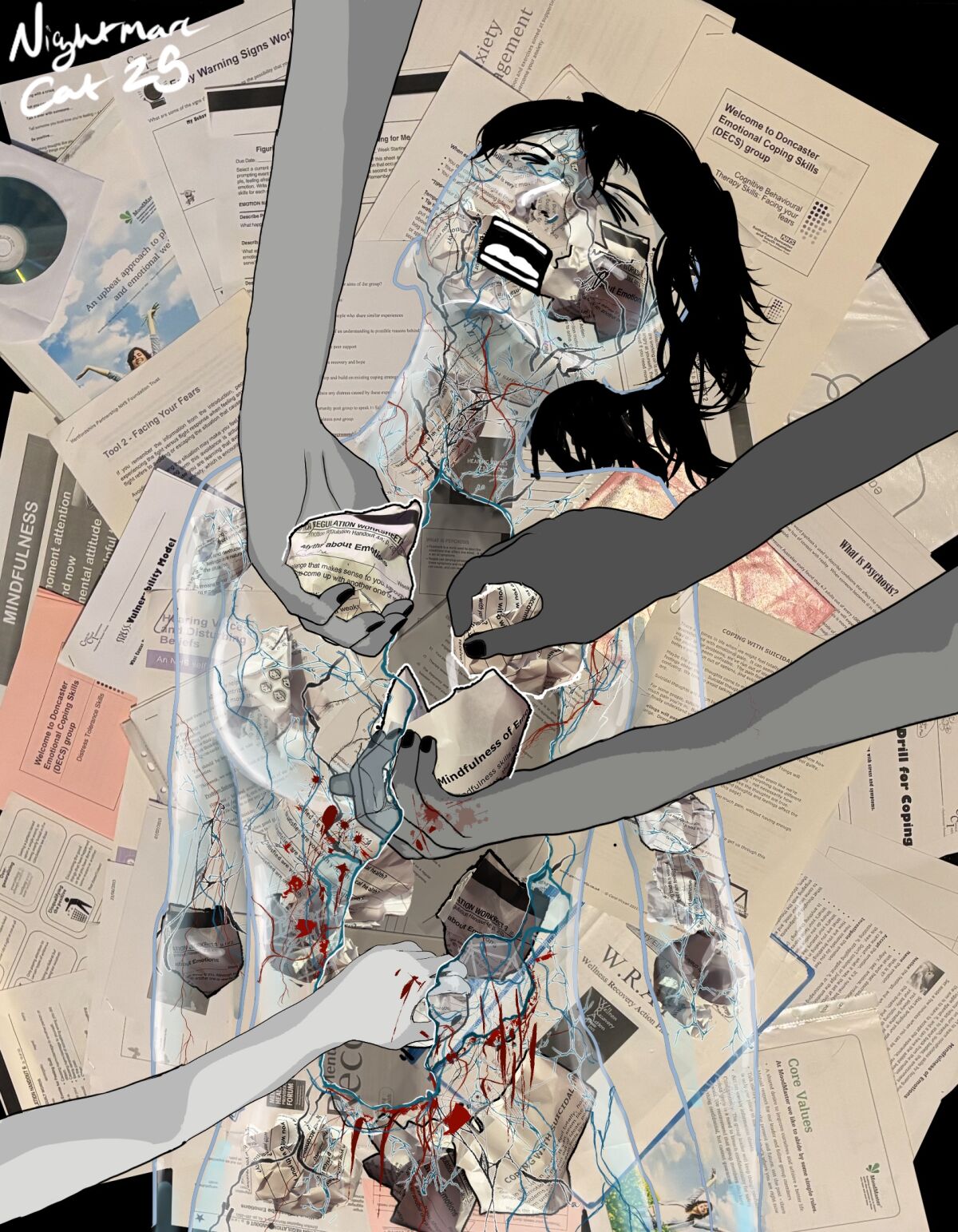
The mental health team currently have me down for therapy, which I’ve asked for adaptations. I’ve been in the system now for a while, and I’ve not taken much in enough that I’ve started to make artwork out of the piles of therapy paper piled up. I don’t learn the traditional, read, write, listen to way. Bad enough, a teacher at my primary school had me investigated for petite mal epilepsy, I’m a practical learner, I’ve handed over my educational assessment done at my university to the Mental health team around 3 times, that states the adaptions the university had to make, which those adaptions got me from a prediction of a 3rd without to honours to a 2:2 however, I’ve been told the team’s adaptions will be fidget toys and it will be a small group, Which yes that might do some autistic people. But not everyone with autism is the same. The service needs to start listening to what its patients need. And not just threatening to discharge, which is what I’m getting, if you don’t fit in their box. Professionals need to understand that autism is a spectrum; what is good for one autistic person isn’t necessarily good for another.
RDaSh talks about person-centred care; however, if it were that, you’d think there would be less of a conveyor belt system and more of a personalised care system. Instead, it’s more focused on diagnosis and kicking you out.
I have a name.
I’m more than my diagnosis.
So many times I bring up my needs to be in a mental health service, and I get the reply about funding, sure, I get it, I’m disabled. It costs a lot. And things are likely to get worse.
Compared to the past decade, the People Focused Group (PFG) has been offering me more actual person-centred support and a place to rant about the mental health team. They gave me a place where I didn’t have to feel alone in all of this. They were the ones who called the ambulance at the end of February when the community mental health team and crisis team dismissed me again and they validated me at the Hearing Voices group. They’ve also helped me grow by including me in the learning disability group Choices for all Doncaster - Chad, and encouraging me to volunteer at Safe Space, which is hopefully my next goal, and inspiring me to do my artwork.
The publisher is Citizen Network. My Name is Cat Wood © Cat Wood 2025.
Illustrations © Cat Wood 2023
community, disability, Inclusion, mental health, Peer Support, England, Article